Time in range (TIR) can help healthcare providers (HCPs) and people with diabetes (PWD) understand their glucose on a deeper level. People with diabetes’ glucose levels can change from day to day—since time in range can help analyze patterns, prepare for different parts of life, and give grace and context to numbers, it’s an incredible tool that’s helping people feel less frustrated about exercising!
For those using continuous glucose monitoring (CGM) systems, glucose TIR is a metric that many HCPs and PWD are benefiting from. The American Diabetes Association (ADA) standards of care1 and CGM consensus guidelines2 recommend a goal of TIR >70% in people with diabetes using CGM.
Reasons why exercising is so important for people with diabetes
Regular movement, physical activity, and exercise are essential for every—for ALL people with diabetes. Exercise has numerous health benefits, including:
- increases in insulin sensitivity
- improvements in TIR
- reduced cardiovascular disease risk
- improvements in weight management and body composition
- strengthens muscles and bones (particularly in youth)
- supports mental health and well-being
- improves overall cardiovascular health
- and reduces the risk of long-term complications.4
Whether it is type 1 diabetes (T1D), type 2 diabetes (T2D), pediatric or adult data, evidence suggests that acute (single sessions) or regular exercise leads to increases in TIR.
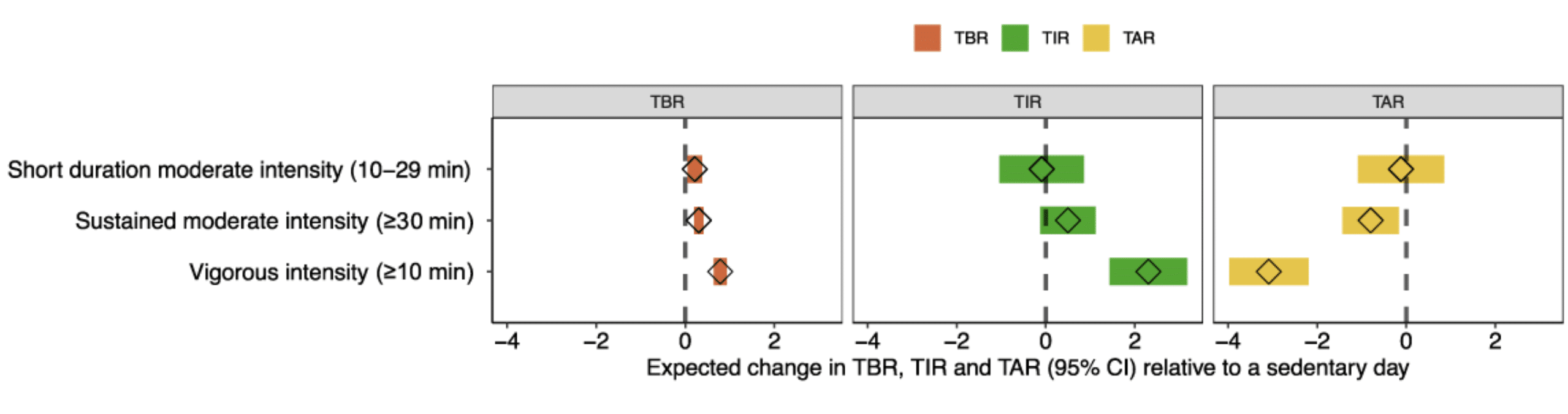
Riddell et al. demonstrated that 24-hour mean glucose and TIR increased on exercise days compared to sedentary days in adults with T1D.5 Similarly, Zaharieva et al. recently showed that youth with new onset T1D had significant increases in TIR in the 24-hours following exercise compared to sedentary days (Figure 1).6 Pemberton et al. nicely reported in adult and pediatric T1D data that 10–30 minutes of moderate-to-vigorous intensity activity within four hours of an insulin bolus and when glucose levels are between 180–250 mg/dL is a safe strategy for increasing TIR.7 Zhu et al. also showed that compared to control (no exercise) interventions, physical activity interventions were associated with significant decreases in glucose variability and increases in TIR in both T1D and T2D.8
How time in range is changing the game
As we know, glucose levels change day to day for PWD, for a variety of reasons. However, TIR can be a helpful metric in so many ways. For example, TIR can:
Show how current routines are working or need adjusting
TIR gives a nice picture of day-to-day glycemic patterns around exercise, and this can help HCPs and PWD identify what is going well and what may need adjusting.
Demonstrate possible patterns
Over time, TIR patterns may begin to appear when looking at CGM data. For example, exercise in many instances causes glucose levels to drop. HCPs and PWD can look at exercise days compared to sedentary days as a tool to highlight potential patterns or differences in TIR.
Be used as a guide for safe exercise
Reviewing glucose values and TIR can be a helpful way to determine safe starting values for exercise. For example, for adolescents with T1D, if glucose levels are between 130-160 mg/dL, research has shown this is generally a safe place to start exercise and minimize the risk of hypoglycemia or hyperglycemia.3
Help to evaluate diabetes management strategies
Using TIR, HCPs and PWD can evaluate whether adjustments in insulin, medication, meal timing, or exercise type/intensity/duration are needed to increase confidence around activity.
Support shared decision-making
HCPs should always consider the goal of PWD first and foremost. Is the goal of the PWD to increase daily steps, build muscle, lose weight, or optimize performance for a specific sport? Using TIR, HCPs and PWD can work together to create exercise strategies based on actual CGM data.
Individualizing care is essential
One thing is certain—not every PWD responds the same way to exercise! Not only do we see individual differences in PWD from one day to the next, but we also know that differences exist between PWD.
As such, for HCPs, individualizing care in PWD is critical. Glucose responses to exercise vary widely, even within the same person. TIR can help reveal each individual’s unique patterns rather than over-generalizing across a whole population.
Factors such as baseline fitness, previous hypoglycemia, insulin on board, exercise type, intensity, and duration can all lead to variability in glucose responses.
Overall, glucose responses to exercise can differ drastically both between and within PWD, so individualizing care is essential in T1D and T2D. TIR gives HCPs a clearer window into each person’s unique patterns by capturing how factors like fitness, recent hypoglycemia, insulin on board, and exercise type influence glucose during exercise.
Get started with TIR in practice today with this free HCP diabetes technology toolkit.
References
- American Diabetes Association Professional Practice Committee. 6. Glycemic Goals and Hypoglycemia: Standards of Care in Diabetes-2025. Diabetes Care. 2025;48(1 Suppl 1):S128-S145. doi:10.2337/dc25-S006
- Battelino T, Danne T, Bergenstal RM, et al. Clinical Targets for Continuous Glucose Monitoring Data Interpretation: Recommendations From the International Consensus on Time in Range. Diabetes Care. 2019;42(8):1593-1603. doi:10.2337/dci19-0028
- Bergford S, Riddell MC, Gal RL, et al. Predicting Hypoglycemia and Hyperglycemia Risk During and After Activity for Adolescents with Type 1 Diabetes. Diabetes Technol Ther. 2024;26(10):728-738. doi:10.1089/dia.2024.0061
- Chimen M, Kennedy A, Nirantharakumar K, Pang TT, Andrews R, Narendran P. What are the health benefits of physical activity in type 1 diabetes mellitus? A literature review. Diabetologia. 2012;55(3):542-551. doi:10.1007/s00125-011-2403-2
- Riddell MC, Li Z, Beck RW, et al. More Time in Glucose Range During Exercise Days than Sedentary Days in Adults Living with Type 1 Diabetes. Diabetes Technol Ther. 2021;23(5):376-383. doi:10.1089/dia.2020.0495
- Zaharieva DP, Ritter V, Bishop FK, et al. Physical Activity Is Associated With Improved Glycemic Outcomes in Newly Diagnosed Youth With Type 1 Diabetes: 4T Exercise Program. Diabetes Care. 2025;48(10):1752-1760. doi:10.2337/dc25-0765
- Pemberton J, Li Z, Gal RL, et al. Duration of physical activity required to Ameliorate hyperglycemia without causing hypoglycemia in type 1 diabetes: A T1DEXI adults and pediatric cohort analyses. Diabetes Res Clin Pract. 2025;220:111981. doi:10.1016/j.diabres.2024.111981
- Zhu X, Zhao L, Chen J, et al. The Effect of Physical Activity on Glycemic Variability in Patients With Diabetes: A Systematic Review and Meta-Analysis of Randomized Controlled Trials. Front Endocrinol. 2021;12:767152. doi:10.3389/fendo.2021.767152

